Healthcare Solutions
Healthcare Automation
Solutions
Intelligent & Agentic AI for Healthcare Organizations
Transform revenue cycle and operational workflows, reduce administrative burden, and improve financial performance with intelligent automation. Zeurons AI leverages RPA, AI-assisted decisioning, and agentic workflows to help healthcare organizations automate eligibility, billing, claims, denials, and other high-volume processes.
80%
Efficiency Increases
5x
Faster Turnaround Time
65%
Reduction in Administrative Costs
CUSTOMER STORIES
Every Success Story Starts With a Vision
Our customers inspire us every day. It’s our privilege to help them achieve their goals and reimagine what’s possible.
There is no question in my mind that without Zeurons AI, we certainly wouldn’t be where we are today.
Zeurons AI developed bots and a full automation framework that reduced manual effort, improved accuracy, and enhanced productivity. They integrated OCR technology and automated complex SAP processes, delivering structured sprints, transparent communication, and on time outcomes.
Rhea Kagan
Revenue Cycle Management, Community Hospital
Community Hospital
INDUSTRY:
Heathcare providers
TECHNOLOGIES:
Intelligent Automation, Workflow Automation, RPA
Healthcare Automation Solutions
Healthcare automation refers to the use of intelligent automation technologies — including RPA, AI, and workflow orchestration — to streamline high-volume operational processes across healthcare organizations.
Revenue cycle automation is the most common entry point for healthcare automation initiatives. These workflows are high volume, highly manual, and directly tied to financial performance, making them ideal candidates for intelligent automation.
Eligibility & Benefits

Eligibility Verification
Real-time insurance coverage checks, deductibles, coinsurance, copay extraction, out-of-network checks, and plan effective/termination dates.
Benefits Interpretation
Category-level benefits, CDT/CPT-specific benefit extraction, frequency limits, exclusions, and waiting periods.
Coordination of Benefits (COB)
Primary vs secondary validation and automatic COB update suggestions.
Systems & Tech Stack
- Availity
- Change Healthcare
- NaviNet
- Epic
- Cerner
- Athenahealth
#EligibilityVerification #BenefitsExtraction #EDI270271 #PayerPortalWorkflows #HealthcareRPA
Prior Authorization
Accelerate authorizations by automating data gathering, submission, status checks, and payer documentation requirements using AI agents and RPA with EMRs and payer portals.

Is Authorization Required?
Procedure-to-payer rules engine and CPT/ICD requirement check.
Document & Data Gathering
Clinical note extraction (visit notes, imaging, labs) and medical necessity criteria matching.
Submission & Status Monitoring
Portal-based submission, API/EDI submission where available, and real-time status check & updates.
Systems & Tech Stack
- Availity
- CareFirst
- Aetna
- Optum
- eviCore
- Epic
#PriorAuthorization #eviCoreAutomation #AIMPortal #MedicalNecessity #PayerSubmissionBot
Claims & Billing
Improve clean claim rates and speed up payment posting by automating coding checks, claim creation, charge capture, and billing processes.

Charge Capture
Pulling charges from EMR, mapping CPT + modifiers, and validating missing information.
Claim Creation
CMS-1500 & UB-04 generation, payer-specific edits, and batch submission logic.
Payment Posting
ERA/EOB reading, auto-post to PM/EHR, and variance & underpayment detection.
Systems & Tech Stack
- Availity
- Change Healthcare
- Waystar
- Epic Resolute
- Kareo
#MedicalBillingRPA #ClaimsSubmissionBot #ERAAutomation #ChargeCaptureAI #RevenueCycleAI
Denials & Appeals
Recover missed revenue by automating denial identification, classification, root-cause analysis, and appeal preparation.

Denial Identification
Auto-read CARC/RARC from EOB/ERA and categorize into reasons (authorization, coding, eligibility, missing info).
Prioritization & Routing
Sort by financial impact and predictive likelihood of overturn.
Appeals Creation
Auto-generate appeal letters, attach supporting clinical docs, and submit to payer portal.
Systems & Tech Stack
- Availity
- Waystar
- Epic Resolute
- Athenahealth
- NextGen
#MedicalBillingRPA #ClaimsSubmissionBot #ERAAutomation #ChargeCaptureAI #RevenueCycleAI
Patient Access
Streamline front-desk and onboarding processes by automating intake, registration, scheduling, demographic validation, and insurance capture.

Patient Registration
Automated demographic import, ID & insurance card scanning, and duplicate patient detection.
Scheduling & Check-In
Appointment slot optimization, automated reminders, and no-show risk predictions.
Financial Clearance (Front-End RCM)
Estimation of patient responsibility, payment plan eligibility, and copay collection reminders.
Systems & Tech Stack
- Epic Welcome
- Athenahealth
- Phreesia
- SolutionReach
- NexHealth
#PatientIntakeAutomation #DigitalFrontDoor #PatientAccessAI #SelfRegistration
Clinical Workflows
Reduce clinician and admin burden by automating repetitive documentation, order entry, routing, and operational workflows.

Clinical Documentation Support
Extracting structured fields from notes, clinical document classification, and auto-generation of visit summaries.
Order Management
Lab & radiology order entry, monitoring order status, and result triage & routing.
Operational Workflows
Bed utilization support, staff scheduling, and census reporting.
Systems & Tech Stack
- Epic
- Cerner
- Meditech
- Allscripts
- LIS
- RIS
#ClinicalWorkflowAutomation #EHRDataEntry #OrderEntryBot #DocumentationAI
Patient Communications

Intelligent Routing
Routing based on intent, insurance status, and clinical urgency.
Appointment Support
Automated scheduling/rescheduling, reminder calls & SMS, and pre-visit instructions.
General Inquiries & Self-Service
Benefit questions, directions, hours, forms, and payment balance inquiries.
Systems & Tech Stack
- Availity
- CareFirst
- Aetna
- Optum
- eviCore
- Epic
#HealthcareContactCenterAI #PatientCommunication #MedicalVoicebots #AppointmentChatbot
Benefits of Intelligent Automation & RPA in Healthcare
Increased Revenue Cycle Efficiency
Streamline claims, billing, and insurance verification with intelligent RPA and automation. Reduce denials, speed up reimbursements, and ensure accurate coding—boosting your entire revenue cycle—boosting financial performance for your hospital or clinic.
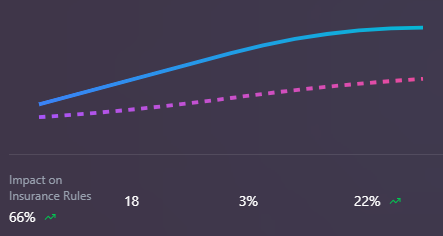
Revenue Cycle Inefficiencies
Manual processes result in delayed claims, high denial rates, and significant revenue leakage.
Unified Patient Data & Workflow Integration
Centralize access to patient records, clinical documentation, and test results through secure healthcare automation platforms. Improve care coordination, enable data-driven decision-making and deliver integrated, connected care for every patient.
Advanced Compliance & Data Security
Maintain HIPAA compliance and protect PHI with automated audit trails, real-time monitoring, and strict access controls. Healthcare automation ensures regulatory standards are met while minimizing risk and preventing unauthorized data access.
Enhanced Patient Engagement
Empower patients with self-service portals for appointments, access to medical records, and real-time communication. Reduce wait times, improve satisfaction, and enable seamless engagement with healthcare teams using automated, user-friendly tools.
Faster, More Accurate Diagnostics
Integrate data analytics and AI to deliver rapid test results and actionable clinical insights. Reduce delays and data entry errors, giving clinicians and patients faster access to diagnostics and improving clinical outcomes across the board.
KEY BENEFITS OF A DIGITAL WORKFORCE
Refocus on Patients with Faster Operations
Imagine a world where your teams don’t need to spend their time facilitating tedious, error-prone processes and your patients enjoy faster, more personalized experiences. It’s all possible when you automate routine processes and tap into AI’s potential for tasks that make staff feel more “robot” than human.
Improve Administrative Workflows
Automate repetitive administrative tasks, freeing staff to focus on high-value activities that improve patient care and operational efficiency.
Enhance Clinical Documentation
Reduce documentation burden with AI-powered assistants that capture, validate, and structure clinical notes automatically
Combat Caregiver Burnout
Empower healthcare teams by removing tedious tasks, allowing them to spend more time with patients and reduce stress.
Maintain Compliance with Confidence
Ensure HIPAA compliance and regulatory standards with automated monitoring, audit trails, and secure data management.
Automate Up To 90% of Revenue Cycle
We offer artificial intelligence-powered solutions that can be customized and retrofitted into your current infrastructure. This way we are able to maximize your outcome through optimization of your current resources.
Use Cases
Healthcare Automation
Across the Continuum
💰
Revenue Cycle Management
Automate claims processing, billing, and payment reconciliation to reduce errors and accelerate cash flow.
📋
Patient Intake & Scheduling
Streamline patient registration, appointment scheduling, and pre-visit documentation with intelligent automation.
📝
Clinical Documentation
Reduce clinician burden with AI-powered documentation assistants that capture, structure, and validate clinical notes.
✅
Prior Authorization
Accelerate prior auth approvals with automated submission, tracking, and follow-up workflows.
🔄
Claims Denial Management
Predict, prevent, and resolve claim denials with AI-driven analytics and automated resubmission.
🛡️
Compliance & Audit
Ensure HIPAA compliance and audit-readiness with automated monitoring, reporting, and documentation.
Empowering Healthcare Providers
with Intelligent Automation Solutions
Transform your healthcare operations with Zeurons AI’s end-to-end automation portfolio. Our solutions help providers streamline clinical and administrative workflows, boost patient care, and achieve operational excellence across every department.
Revenue Cycle Automation for Providers
Automate end-to-end RCM processes to accelerate cash flow and reduce denials.
01
- Authorization and claim status checks
- Scheduling and reminders
- Health information management (release of information, care documentation)
- Claims management
- Insurance verification
- Coding and charge capture
- Cash posting and reconciliation
Finance and Accounting Automation
Optimize accounts payable, receivable, and reporting with intelligent workflows.
02
- Accounts payable and invoicing
- Data collection, reporting, and analytics
- Accounts receivable and reconciliation
IT and Clinical Operations
Drive efficiency in IT support, clinical documentation, and patient scheduling.
03
- Enterprise testing, help desk, support, and migrations
- Clinical documentation automation
- Patient screening and scheduling
- Password reset and user management
- Epic InBasket, registry updates
Credentialing, Enrollment, and Contracting Automation
Streamline payer enrollment, provider credentialing, and pricing updates.
04
- Fee schedule and pricing updates
- Provider credentialing
- Payer enrollment
Pharmacy and Supply Chain Automation
Ensure compliance and improve supply chain management with automation.
05
- Order intake automation
- Inventory forecasting and ordering
- DUR review and 340b compliance
Technology Stack
Powered by Advanced Automation Technologies
We don’t treat RPA, AI, or analytics as standalone tools. Intelligent automation orchestrates these capabilities together — using RPA for execution, AI for decisioning and exception handling, and analytics for continuous optimization. Intelligent automation allows healthcare organizations to move beyond task automation and toward adaptive, exception-driven workflows that improve over time.
Intelligent Automation
End-to-end process automation
Robotic Process Automation
Task-level automation bots
Workflow Optimization
Process efficiency enhancement
Agentic AI & Machine Learning
Intelligent decision-making
Natural Language Processing
Language understanding & processing
Intelligent Document Processing
Automated data extraction
Ready to Build Smarter Healthcare Operations ?
Accelerate AI adoption in your healthcare organization and enhance operational performance with our tailored solutions.
Contact us today for a free consultation on driving AI-powered transformation that delivers measurable results across your hospital or clinic.